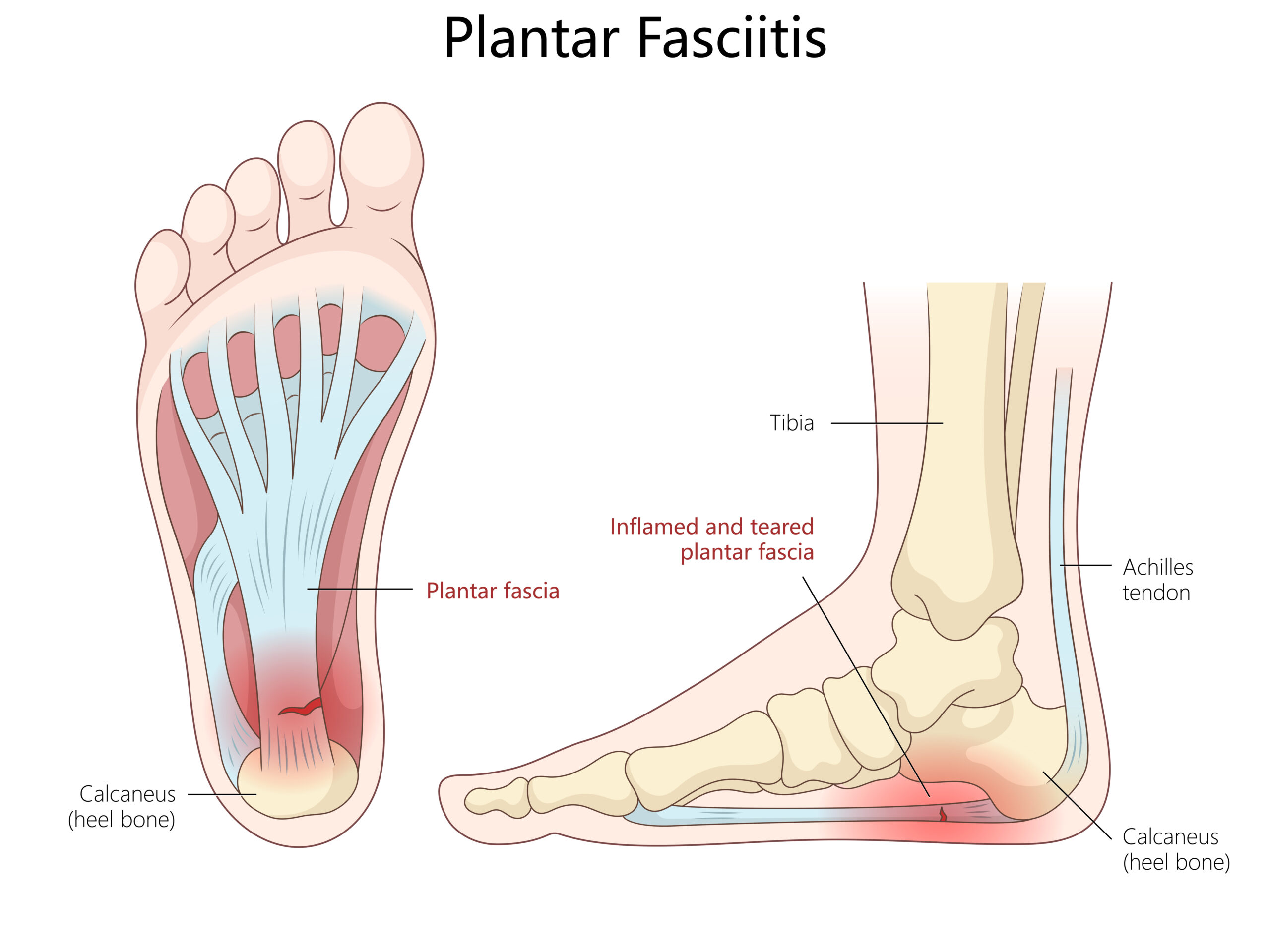
Chronic heel and foot pain isn’t just caused by overuse—it’s often linked to reduced blood flow in the tiny vessels that nourish your foot tissues. When circulation is limited, the plantar fascia and tendons don’t receive enough oxygen and nutrients to heal properly, leading to ongoing inflammation, stiffness, and pain. Conditions like diabetes, poor circulation, or even tight calf muscles can make this worse by restricting blood flow even further. Over time, the tissue becomes thickened and scarred, making each step painful and slowing recovery. The PFE (Percutaneous Fasciotomy and Tenotomy) procedure helps by gently releasing the damaged tissue and improving local circulation. This allows healthy new blood vessels to form, delivering the nutrients needed for real healing. As blood flow and flexibility return, most patients experience less pain, better mobility, and a faster return to daily activity.

Chronic heel and foot pain often develop when the soft tissues that support your foot—especially the plantar fascia and tendons—become overstressed, inflamed, or degenerated over time. These tissues are responsible for absorbing shock, maintaining arch stability, and supporting every step you take. When they are repeatedly strained, microscopic injuries occur faster than the body can heal them, leading to pain and dysfunction.
Daily activities like standing, walking, or running—especially on hard surfaces—can overload the plantar fascia and Achilles tendon.
Over time, the tissue becomes thickened and less flexible, creating microtears that lead to chronic inflammation and scarring.
Flat feet, high arches, or abnormal gait patterns place uneven pressure on the heel and arch.
These biomechanical imbalances strain the fascia and tendons with every step, accelerating wear and tear.
Shoes with inadequate support, thin soles, or worn-out cushioning fail to absorb impact properly.
High heels or unsupportive sandals can alter foot alignment and worsen stress on the fascia.
Extra weight increases the load on the heel and arch with every step, heightening the risk of tissue strain and degeneration.
Tightness in the calf (gastrocnemius) and Achilles tendon limits ankle movement, forcing the plantar fascia to overstretch during walking.
As we age, the collagen fibers in tendons and fascia lose elasticity and strength.
This makes tissues more prone to chronic irritation and slower to heal after injury.
An untreated ankle sprain or repetitive microtrauma can lead to persistent inflammation and scar tissue formation.
Scar tissue restricts normal movement and perpetuates chronic pain.
Patients who are candidates for PFE typically suffer from one or more of the following chronic conditions:
Plantar Fasciitis / Plantar Fasciosis – Persistent inflammation or degeneration of the plantar fascia (the thick band of tissue running across the bottom of the foot).
Achilles Tendinopathy – Chronic pain, stiffness, or microtears in the Achilles tendon that do not respond to conservative care.
Heel Spurs – Bony growths that form where the plantar fascia attaches to the heel bone, often linked to plantar fasciitis.
Post-Traumatic Scar Tissue – Fibrotic tissue following foot or ankle injuries that limits motion and causes pain.
Chronic Foot or Heel Pain Syndrome – Ongoing pain in the heel, arch, or midfoot area lasting more than six months despite non-surgical treatment.
Sharp or stabbing heel pain, especially with the first steps in the morning.
Aching or burning along the bottom or back of the foot after long periods of standing or walking.
Pain that worsens after activity or prolonged rest.
Tightness or stiffness in the heel cord or arch.
Localized tenderness where the plantar fascia or tendon attaches.
Limited range of motion or difficulty performing daily activities due to foot pain.
Before recommending PFE, your provider will perform a thorough evaluation that may include:
Physical Examination – Assessing pain points, flexibility, and gait.
Diagnostic Ultrasound or MRI – To visualize thickened fascia, tendon degeneration, or scar tissue.
Review of Prior Treatments – Such as physical therapy, orthotics, injections, or medications that failed to provide lasting relief.
Patients who have experienced chronic pain for 6 months or longer despite conservative therapies are typically strong candidates for the PFE procedure.
Book your appointment with Heart Vascular & Leg Center
today for personalized care and advanced treatment.





5020 Commerce Drive
Bakersfield, CA 93309
Struggling with PAD symptoms? Our specialists at Heart Vascular and Leg Center are here to help. Schedule an appointment today to see if Varithena is the right solution for you.
Hear from our patients about their experiences at Heart Vascular and Leg Center..

Stay informed with trusted insights on vascular health, PAD prevention, and advanced treatments.
Book your appointment with Heart Vascular & Leg Center
today for personalized care and advanced treatment.
© Copyright 2024 Vascular Health Partners LLC. All Rights Reserved
Designed By CyberWorx